Antibiotics are used to treat bacterial infections. Most antibiotics are “broad-spectrum” antibiotics which means they are active against many types of bacteria. Not only do they act against target harmful bacteria (known as pathogens) but they can also ‘kill’ commensal bacteria. Usually, antibiotics are taken orally which means they can affect our gut microbiota and this can impact on our health.
Impact on the diversity of gut bacteria
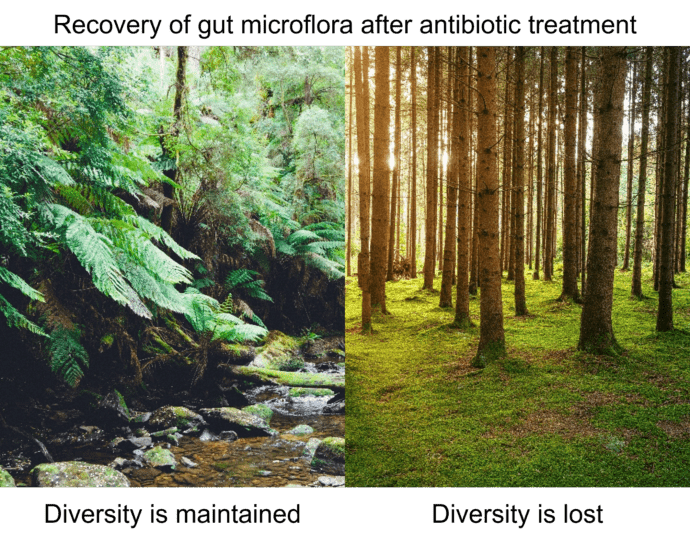
Reduction of the number of bacteria, and number of different bacterial species, within your gut during antibiotic treatment also means that the diversity of gut bacteria is reduced during and immediately following treatment. This may impact on gut health as your gut bacteria work as a consortium. As bacteria live in different locations (different niches) within the gut, some of them will be very exposed to the antibiotics as they pass through the gut while others may be more protected.
In most cases there is quite a quick recovery of a diverse community following the end of treatment as numbers of the bacteria that were protected increase and re-colonise the gut (within one month). Occasionally, certain types (species) of bacteria may be affected long-term, even long after the patient has recovered from the initial infection and has stopped taking antibiotics.
Something else that may happen is that when the normal diversity of the microbiota is decreased, populations of one or two bacterial species that are resistant to the antibiotic can expand and take over. This means that the total number of bacteria might be unchanged, but the diversity within the microbial community is lost.
Antibiotic resistance within the gut
Some bacteria carry genes that make them less susceptible to antibiotic activity. This is called antibiotic resistance and it is a major global concern. When people take antibiotics that affect gut microbes, this can lead to an increase of resistant bacteria which may be harmful. Also, other species of gut bacteria can become resistant by acquiring genes from the resistant bacteria. This can occur through a process called horizontal gene transfer. Even when people have stopped treatment, the recovered community may contain a higher level of resistance genes and this might cause problems in the future.
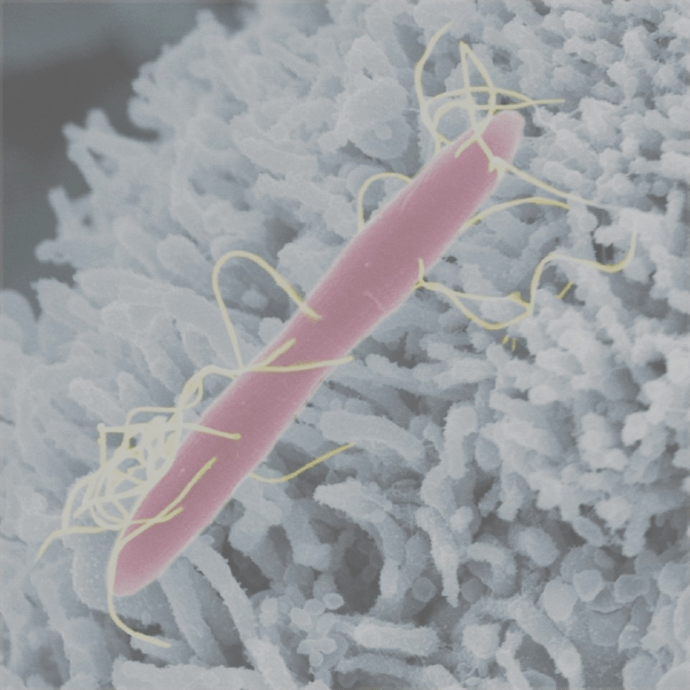
Clostridioides difficile
A serious consequence of the reduction in numbers of healthy host bacteria during and immediately after antibiotic treatment is that it gives pathogens an opportunity to colonise and thrive in the gut. These pathogens can then dominate the community of microbes even once antibiotic therapy has finished. An example of this is Clostridioides difficile, which expands to occupy empty niches following antibiotic therapy.
Overgrowth of C. difficile, which is sometimes referred to as C. diff, results in toxin production, abdominal pain, fever and diarrhoea. C. difficile can form spores which have hard, impermeable coats and are resistant to antibiotics and some C. difficile strains have acquired other antibiotic resistance mechanisms. This can result in recurring C. difficile infections. Sometimes, probiotics are used to treat these infections in intensive care units to reduce the incidence of diarrhoea caused by C. difficile. Faecal microbial transplant therapy is also a successful cure.
Read also

Foodborne pathogens
Antibiotic resistance
Antibiotics are used to treat bacterial infections but bacteria are becoming resistant to these drugs and some infections can no longer be treated.
Gut health
Meet your gut bacteria
Your gut microbiota are very important and do many jobs that keep us healthy but not all microbes that are found in our guts are good for us.